Understanding Image Clarity in Digital Dental Imaging
What Is Image Clarity and Why It Matters in Diagnostic Imaging
The Role of Image Resolution in Clinical Diagnosis
In digital dental imaging, clarity isn’t a luxury—it’s a clinical imperative. High image resolution enables practitioners to discern minute anatomical features, such as incipient carious lesions, periodontal bone loss, or fine endodontic structures. A diagnostically valuable image hinges on the ability to differentiate between subtly varying shades of grey. Without adequate resolution, pathology can hide in plain sight.
How Blur Affects Accuracy and Interpretation of Dental X-rays
Blur acts like a veil over critical data. It obscures edges, blunts contrast, and muddles anatomical delineation. This degradation in sharpness can lead to diagnostic ambiguity, forcing clinicians to rely on inference rather than observation. Inaccuracies here can result in either overtreatment or overlooked pathology—both costly in different ways.
Why Clarity Becomes More Critical in Intraoral and Small-Structure Imaging
The smaller the field, the higher the demand for visual precision. Intraoral imaging—particularly in pediatric, endodontic, and anterior diagnostics—requires exceptional detail. A deviation of even half a millimeter can mean the difference between a healthy root apex and a missed periapical abscess. For small-structure imaging, clarity isn’t optional—it’s foundational.
What Happens with Low-Dose X-rays
The Trade-Off Between Radiation Dose and Image Quality
Dental professionals face a continual balancing act: minimizing radiation exposure while maximizing diagnostic yield. Low-dose protocols emerged from this balancing act, aiming to adhere to ALARA principles (“As Low As Reasonably Achievable”) while still delivering usable imagery. However, this comes at a price.
Common Misconceptions About Radiation Safety vs. Image Performance
There’s a prevailing assumption that any dose reduction is inherently good. But extreme minimization can undercut diagnostic effectiveness. An underexposed image can be more dangerous than a marginally higher dose—it can miss early pathology, leading to delayed treatment or progression of disease.
Regulatory and Patient Safety Pressures to Reduce Exposure
With growing awareness of radiation risks, both regulatory bodies and patients are pushing for exposure reduction. This has driven demand for low-dose systems, often without a parallel understanding of the technical consequences. The result is mounting pressure on imaging systems to do more with less—often exposing the system’s limits.
How Low-Dose Settings Impact Sensor Performance
The Science of Signal-to-Noise Ratio (SNR) in Digital Radiography
At the core of imaging quality is the signal-to-noise ratio. In low-dose scenarios, the number of X-ray photons reaching the sensor drops. Fewer photons translate into lower signal strength, while electronic noise remains constant. The result is a compromised SNR, manifesting as blur or a grainy, snow-like texture on the image.
How Fewer Photons Mean Less Data for Image Construction
Imaging is a data-driven process. With fewer photons captured, the image processor has less raw information to construct a coherent visual output. This forces the software to interpolate, smooth, or extrapolate—techniques that inherently dilute image sharpness and may introduce artifacts.
Clinical Symptoms of Underexposure: Blur, Graininess, and Missed Pathology
Underexposure isn’t always obvious to the untrained eye, but its signs are there: fuzzy margins, uneven contrast, blotchy textures, and diagnostic blind spots. In worst-case scenarios, early caries, root fractures, or marginal bone changes can go undetected until they become more severe—and harder to treat.
Not All Sensors Are Created Equal
How Dynamic Range and Sensitivity Vary Across Sensor Types
Dynamic range—the sensor’s ability to capture both dark and bright regions simultaneously—is crucial when photon availability is low. Higher sensitivity sensors preserve image contrast and detail even under suboptimal exposure. CMOS sensors with advanced pixel architecture now approach dynamic ranges previously exclusive to CCDs, but not all CMOS units are built equal.
Why Some Sensors Handle Low-Dose Better Than Others
The differentiating factor often lies in quantum efficiency—how effectively a sensor converts incoming photons to a usable electrical signal. Sensors with higher efficiency and lower intrinsic noise preserve clarity even at low doses. Proprietary image-processing algorithms and noise-reduction technologies also give some models an edge, especially in challenging scenarios.
The Role of Sensor Size and Pixel Architecture
How Pixel Size and Layout Affect Spatial Resolution
Smaller pixels capture finer detail, but they also gather fewer photons per unit area—raising the noise floor under low-dose conditions. Larger pixels improve sensitivity but reduce resolution. The ideal sensor strikes a balance between pixel size and layout geometry, often using microlenses or enhanced fill factors to optimize photon capture.
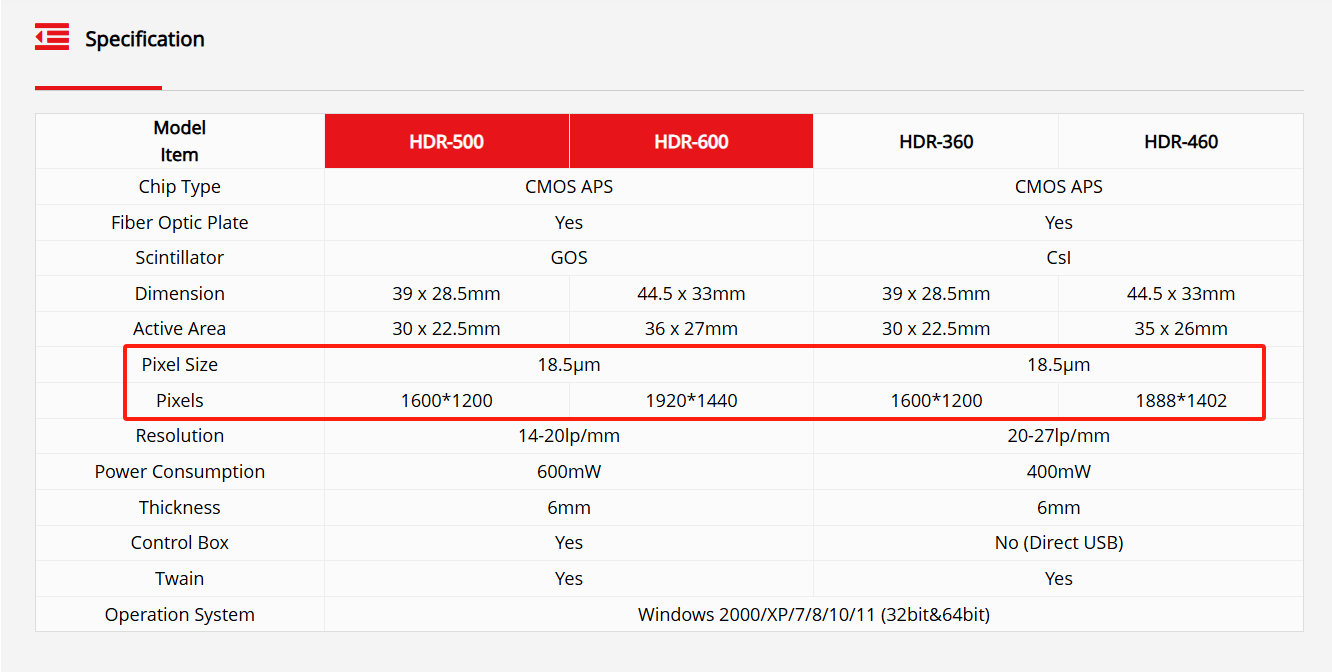
Our sensors are engineered to achieve this balance precisely. With an optimized pixel size of 18.5μm, they provide both high sensitivity and fine spatial resolution—ensuring clear imaging even under reduced radiation settings. Combined with tailored sensor configurations such as 1600×1200, 1920×1440, and 1888×1402, this architecture supports accurate diagnostics across a variety of clinical use cases without compromising image quality at low doses.
What “Micron Level” Differences Really Mean for Practitioners
It’s tempting to dismiss a difference of 1–2 microns as negligible. However, in a diagnostic context, these tiny increments can define the edge between observing a microcrack and missing it entirely. Micron-scale refinements often translate into meaningful clinical precision, especially in restorative planning and root canal evaluations.
The Hidden Influence of Internal Noise and Conversion Efficiency
Even with optimal pixel size, internal electrical noise can sabotage clarity. Poor analog-to-digital conversion (ADC), thermal noise, or suboptimal shielding can degrade the final image. A sensor’s technical data sheet may not list these factors, but in real-world use, they become apparent quickly.
When Blur Isn’t Just About Dose
Poor Calibration, Aging Equipment, and Other Technical Pitfalls
Sensors degrade with time—just like any other piece of technology. Wear and tear, exposure to moisture, or repeated sterilization cycles can alter a sensor’s responsiveness. Additionally, firmware mismatches or outdated drivers can impair performance. Routine calibration is essential to maintain consistent clarity and eliminate non-dose-related blurring.
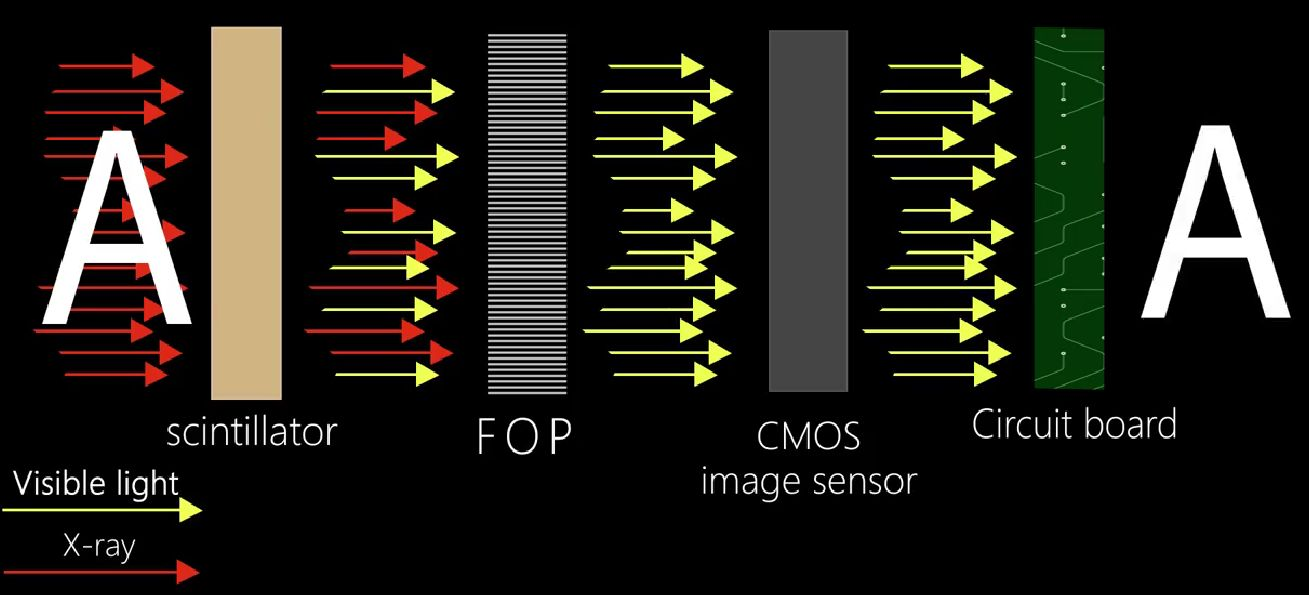
To address these long-term challenges, our sensors are equipped with a built-in Fiber Optic Plate (FOP), which acts as a protective barrier against residual X-ray radiation. By filtering out high-energy rays that typically contribute to internal sensor wear, the FOP not only reduces radiation-related damage but also significantly extends the device’s operational lifespan—helping maintain clarity and reliability over time.
Importance of Regular Sensor Calibration and Software Updates
Calibration aligns the sensor’s response to real-world exposure levels. Without it, even a well-made sensor can underperform. Likewise, imaging software evolves to better interpret sensor signals and correct noise. Neglecting updates can mean relying on outdated processing protocols—effectively blunting a modern sensor’s capabilities.
Common Maintenance Oversights That Can Reduce Image Clarity
Dirty lenses, improperly stored sensors, and unshielded cables can introduce avoidable artifacts. Even cable kinks can affect data transmission, subtly degrading image output. Routine inspections and basic hygiene protocols can go a long way in protecting diagnostic integrity.
Positioning, Movement, and Human Error
The Impact of Patient Motion on Low-Dose Clarity
Even minor shifts during exposure can blur fine details. At low doses, where image acquisition is more sensitive to signal loss, the margin for error narrows dramatically. Pediatric and geriatric patients are particularly prone to movement, necessitating extra precautions.
Operator Technique: How Sensor Placement Affects Image Fidelity
Angulation, pressure, and sensor positioning all influence image geometry. An improperly aligned sensor can cause distortion, elongation, or shadowing—effects that become pronounced under low-dose settings. Experienced technique remains a key countermeasure to low-dose limitations.
Tips for Minimizing User-Based Causes of Blurring
Use bite blocks to stabilize positioning. Offer verbal reassurance and breathing cues to reduce patient movement. Confirm software settings match the sensor in use. Such simple interventions can dramatically enhance image consistency, especially in high-volume practices.
Choosing the Right Tools for the Job
What to Look for in a Sensor Built for Low-Dose Performance
High sensitivity, low-noise architecture, and robust signal processing should top the list. Beyond specs, look for real-world image samples across various exposure levels. Advanced models incorporate smart algorithms that adapt in real time to exposure changes, optimizing clarity automatically.
Sensors with a wide dynamic range are especially advantageous. This capability allows the system to handle both low- and high-dose exposures with consistent image quality, minimizing the chance of retakes and reducing clinical workflow friction. By accommodating variable shooting conditions, these sensors help ensure high-resolution, diagnostically useful images—regardless of dose settings.
Handy Medical sensor’s wide dynamic range enables consistently sharp images at both low and high doses, helping clinics reduce film waste and increase diagnostic accuracy.
Case Studies or Test Images: How to Evaluate Sensor Performance in Real-World Settings
Before investing, request test images taken at reduced dose settings. Compare resolution across difficult-to-capture areas—apices, interproximal spaces, or the mandibular molar zone. A good sensor should maintain fidelity across variable scenarios, not just in ideal test environments.
Balancing Dose Reduction with Diagnostic Confidence
When It’s Worth Using Standard Dose Over Ultra-Low-Dose Modes
Some cases demand precision over prudence. Pre-surgical assessments, endodontic diagnostics, or suspected fractures often warrant standard-dose imaging. Pushing ultra-low protocols universally can compromise patient care. Dose strategy should be contextual, not dogmatic.
How to Tailor Dose Settings to Patient Profiles and Clinical Scenarios
Use age, anatomy, and clinical purpose as guideposts. A routine recall in a healthy adult may tolerate a lower dose; a symptomatic child with erupting molars may not. Dynamic dose customization—supported by preset protocols—is increasingly common in modern practices.
Educating Patients: Communicating the Safety–Clarity Balance Professionally
Patients often equate “less radiation” with better care. Clinicians must reframe the conversation: “We minimize exposure, but we prioritize accurate diagnosis.” Transparent, jargon-free explanations foster trust and understanding—especially when opting for higher-dose imaging is the safer path.
Optimizing Your Practice for the Next Generation of Imaging
Updating Protocols for Better Low-Dose Outcomes
Modern imaging demands modern protocols. Regularly audit imaging results, calibrate machines, and update exposure guidelines to match your equipment’s evolving capabilities. Continuous refinement ensures patients benefit from both safety and precision.
Staff Training and Patient Education as Strategic Advantages
Technology is only as good as its operator. Invest in continuing education and technical training for your team. A confident, informed staff not only delivers better images—they also build patient trust and reduce retakes.
Investing in Longevity: How to Future-Proof Your Diagnostic Workflow
As imaging systems evolve, so should your infrastructure. Choose scalable software, modular hardware, and vendors with clear roadmaps for innovation. Future-proofing isn’t about chasing trends—it’s about making deliberate, informed choices that sustain clarity, compliance, and clinical excellence.
Post time: May-09-2025